Automated Vertebral Fracture Assessment


|
Project ParticipantsThe current participants in this project at the Centre for Imaging Sciences are:
This project is funded by the ARUK - Arthritis Research UK |
|||||||||||||||||


|
OverviewThis project seeks to develop reliable automatic methods of detecting and classifying vertebral fractures by measuring the shape and appearance of vertebrae in radiographs and both dual and single energy X-ray absorptiometry (DXA and SXA) images of the spine. Detection of vertebral fractures is important for the early diagnosis of osteoporosis, and for clinical trials of osteoporosis treatments. Current vertebral classification methods will be extended by using the full shape and appearance, rather than a small subset of height information. One output will be an analysis tool to be made available to collaborating researchers and clinicians. Our current accuracy results on DXA images are as good as manual precision on normal vertebrae, and within manual precison on around 85% of fractured vertebrae. Reliable results are obtained even on severely fractured vertebrae. |
|||||||||||||||||

|
Context - OsteoporosisOsteoporosis is one of the most important diseases facing the elderly, and as life expectancy increases, this makes it a serious public health problem. There are around 200,000 osteoporotic fractures per year in the UK, and more than 40% of middle-aged women in Europe will suffer such fractures during their remaining lifetime. Osteoporosis is one of the most expensive chronic diseases, and its cost is increasing rapidly. In the EU osteoporosis now costs more than 4.8 billion Euros annually in hospital healthcare alone, a 33% increase over three years, whilst in England and Wales, the total direct hospital cost of osteoporotic fractures in 1999 was �584 million. Postmenopausal osteoporosis is a significant cause of morbidity and mortality amongst the elderly in the Western world, leading to large numbers of fractures of the hip, spine and wrist. Hip fractures are the most serious and painful: 27% of women who sustain a hip fracture die within 1 year. Half of all osteoporotic fractures are vertebral: a 50 year old woman has a one in four chance of having such a fracture, a 50 year old man about half that risk. Vertebral fractures tend to occur about two decades earlier than hip and other osteoporitic fractures, and are often the first clinical sign of osteoporosis. The presence of even one vertebral fracture increases the risk of any subsequent vertebral fracture five-fold, and the risk of a subsequent hip fracture is doubled. In trials of new treatments for osteoporosis, incident vertebral fracture statistics are studied, and used as a measure of efficacy. For patients with vertebral fractures proven therapies are available which reduce the incidence of subsequent fractures by 50% or more . All such patients need treatment, as the risk of further fractures is high, around 20% in the 12 months following a recent vertebral fracture. Thus early detection is important. |
|||||||||||||||||

|
Project GoalsThe key goals of the project are to:
|
|||||||||||||||||
|
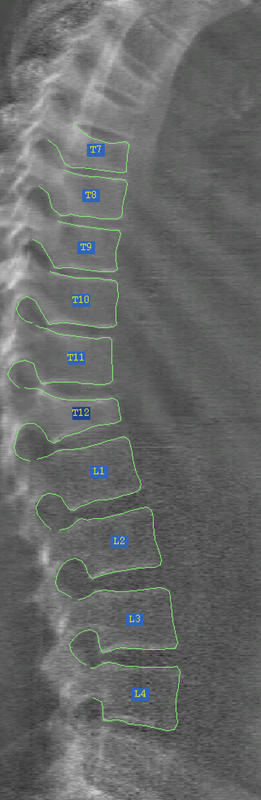
MethodologyAutomatic Location of VertebraeThe core automatic morphometry is built upon ISBE's existing computer vision software , such as the Active Shape Model (ASM) and the Active Appearance Model (AAM). These are well-established in coping with the difficulties of medical images, such as noisy and incomplete data. Statistical shape models are robust in the presence of image noise, as the generated shape always remains within physically reasonable bounds learnt from the training set; and since correlations between different sub-parts are modelled, the approximate location and shape of any obscured portions can be inferred from other parts. |
|||||||||||||||||
|
|
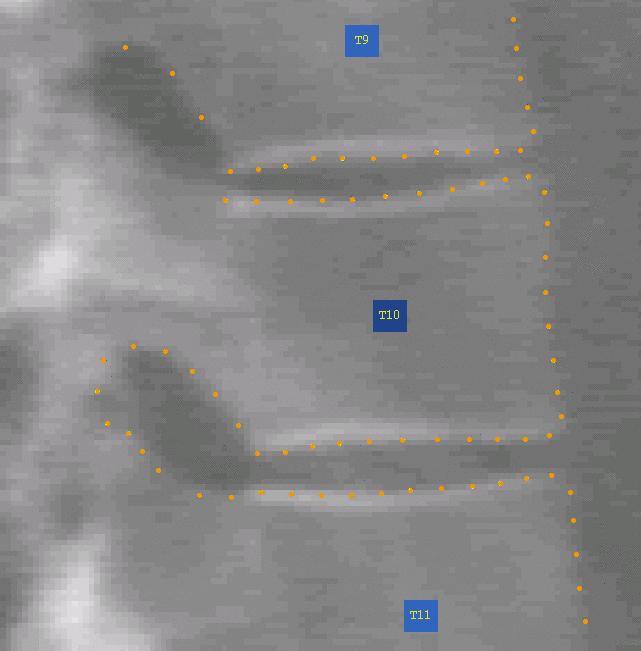
Initial results show that modelling the whole spine as a single (deformable) structure leads to good matching for normal vertebrae. However, the range of variability in fractured vertebrae would pose a problem for a global model. Not only can individual fractured vertebrae vary in a much wider manner than normal ones, but there may be combinations of fractured vertebrae not present in the training set. Also conditions such as scoliosis can shift vertebrae out of their normal alignment. Thus the global model is likely to be over-constrained. It is more feasible to build models of smaller portions of the spine, including fractured examples in the training set for each vertebra. However, these models must then be combined together to ensure overall consistency. Our approach is to use overlapping triplets of vertebrae. The overlapping portions link the various sub-models together using point constraints, incorporated as priors in a Constrained AAM fit. The overlaps also assist in the initialisation of the next triplet sub-model for the next iteration. This feed-forward of linking constraints is further assisted by re-performing a weighted least squares fit of a global shape model of the whole spine after each sub-model triplet iteration. Thus the next vertebrae on can be predicted, and soft constraints attached to this prior also. The ordering of the sequence of models is dynamically adjusted to defer any poorly fitting regions until they are constrained by neighbours. This gives good robustness against noise. Location Accuracy ResultsAccuracy results on DXA are as good as manual precision on normal vertebrae (mean accuracy c. 0.7mm, 95% of points within 2mm), and within manual precision limits of 2mm on around 90% of fractured vertebrae (mean accuracy 0.96mm). However further training is needed for the most extreme of severe fractures. We are also researching how to avoid local minima in the case of fractured vertebrae. For example the AAM may fit the top of a severely fractured vertebra onto the bottom edge of the vertebra above (or vice versa), if the fracture has collapsed the edge of the endplate too far from the initial solution. Thus it is necessary to provide several alternative initialisations and select the best one. This has reduced such failure modes. |
|||||||||||||||||
|
|
Classification of vertebraeCurrent quantitative morphometric methods of vertebral fracture detection lack specificity, particularly with mild fractures. We have used more detailed shape and texture information to develop quantitative classifiers. The appearance models used for the automatic segmentation provide a compact means of capturing detailed shape and texture information about a whole vertebrae. We have selected relevant subsets of shape and appearance parameters using stepwise regression, and trained linear discriminants on both the shape and overall appearance parameters.Classification ResultsThe appearance-based classifiers gave better specificity than shape-based methods in the lumbar and mid-thoracic spine. The specificity was 95% at a sensitivity of 95%, representing a sensitivity of 85% on grade 1 fractures (vs 65% for height ratio morphometry), and 98.5% on grade 2 or 100% on grade 3. The main improvement was in the detection of mild fractures. This work has been published in Academic Radiology. We have also evaluated the appearance classifier performance on vertebrae which were segmented automatically using the Active Appearance Model methodology. There is a modest reduction in accuracy due to some segmentation errors in the automatic method. The sensitivities at 2.5% or 5% False Positive Rate respectively are: 78%, 86% (appearance); compared to 66%, 75% with standard morphometry. The appearance classifier can distinguish between true vertebral fractures and other short vertebral height deformities more reliably than height-based methods. This work has been publishe in Osteoporosis International. |
|||||||||||||||||
|
Imaging ModalitiesOur initial work has been on DXA images. We are currently extending our modelling to include radiographs (both thoracic and lumbar). We have recently obtained promising results (mean accuracy 0.64mm) on lumbar radiographs with an accuracy similar to DXA on a dataset of over 500 digitised lumbar radiographs, despite the projective parallax and tilting ("bean-can effect") of the fan X-ray beam. This work has been published in Osteoporosis International. We are also actively working on developing shape and appearance models for thoracic radiographs. Classification Texture FeaturesWe are also researching the use of co-occurrence distribution texture features using random forest classifiers to further improve the differential diagnosis between mild osteoporotic fracture and vertebral deformity from other causes such as spondylosis. Fit Success DeterminationWe have also started to use random forest classifiers on image fit residuals to detemine whether an active appearance model convergence was successful or not. This opens the door to selecting the most successful of a number of solutions. |
Papers and Presentations
2003Roberts MG, Cootes TF, Adams JE (2003) Linking sequences of active appearance sub-models via constraints: an application in automated vertebral mnorphometry. In Proc of 14th British Machine Vision Conference; 1:349:358 PDF |
2004Automated Vertebral Morphometry Presentation, UKRC 2004 Roberts MG, Cootes TF, Adams JE (2004) Vertebral Shape: Automatic Measurement using Overlapping Statistical Models of Appearance, (abstract) 10th National Osteoporosis Society Conference, In Osteoporosis International 15:(Suppl 2),S39 |
2005Roberts MG,Cootes TF, Adams JE (2005) Vertebral Shape: Automatic Measurement with Dynamically Sequenced Active Appearance Models. In Proc of 8th MICCAI Conference,2:733-740. Publisher Springer-Verlag Roberts MG, Cootes TF, Adams JE (2005) Automatic Measurement of Vertebral Shape using Statistical Models of Appearance, (abstract) RSNA 2005 Text Here |
2006Roberts MG,Cootes TF, Adams JE (2006) Automatic segmentation of lumbar vertebrae on digitised radiographs using linked active appearance models. In Proc of MIUA Conference 2006 PDF Roberts MG,Cootes TF, Adams JE (2006) Improving the segmentation accuracy of fractured vertebrae with dynamically sequenced active appearance models. In Proc of MICCAI Conference Workshop on joint and bone disease 2006,1-8. Roberts MG,Cootes TF, Adams JE (2006) Vertebral Morphometry: Semi-automatic determination of detailed shape from DXA Images using Active Appearance Models (2006). Investigative Radiology, Dec 2006 41(12):849-59. |
2007Roberts MG, Cootes TF, Pacheco EM and Adams JE. Quantitative vertebral fracture detection on DXA images using shape and appearance models. Academic Radiology (2007) 14:1166-1178. Roberts MG, Cootes TF, Pacheco EM and Adams JE. Quantitative vertebral fracture detection on DXA images using shape and appearance models (presentation). UKRC 2007 PPT Roberts MG, Cootes TF, Pacheco EM and Adams JE. Quantitative vertebral fracture detection on DXA images using shape and appearance models (abstract). National Osteoporosis Society Conference, Edinburgh 2007. Published in Osteoporosis Int 2007 (18 Suppl 3) p19 Poster PPT |
2008Roberts MG, Phd Thesis. Automatic Detection and Classification of Vertebral Fracture using Statistical Models of Appearance. PDF Computer Aided Detection of vertebral fracture using appearance models and a semi-automatic segmentation. Bone Research Society Meeting, Manchester 2008. Poster PPT |
2009Roberts MG, Cootes TF, Pacheco E, Oh T, Adams JE 2009. Segmentation of lumbar vertebrae using part-based graphs and active appearance models.Med Image Comput Comput Assist Interv. 2009;12(Pt 2):1017-24. |
2010Roberts MG, Pacheco E, Mohamkumar R, Cootes TF, Adams JE 2010. Detection of vertebral fractures in DXA VFA images using statistical models of appearance and a semi-automatic segmentation. Osteoporosis Int 2010 Dec;21(12):2037-46. Article |
2011Roberts MG, Oh T, Pacheco E, Mohamkumar R, Cootes TF, Adams JE 2011. Semi-automatic determination of detailed vertebral shape from lumbar radiographs using active appearance models. Osteoporosis Int 23(2) pp.655-664 pp.655-664 {Epub ahead of print}. Article M.G. Roberts, T.F. Cootes and J.E. Adams, "Automatic Location of Vertebrae on DXA Images using Random Forest Regression", Proc. MICCAI 2012, Vol.III, pp.361-368. |